How the clinical inbox burden impacts primary care physicians

Every week, physicians across the country clock hours of administrative work that detract from time with patients—buried in inboxes, reviewing labs, triaging messages, and renewing prescriptions. It’s not just inefficient. It’s demoralizing.
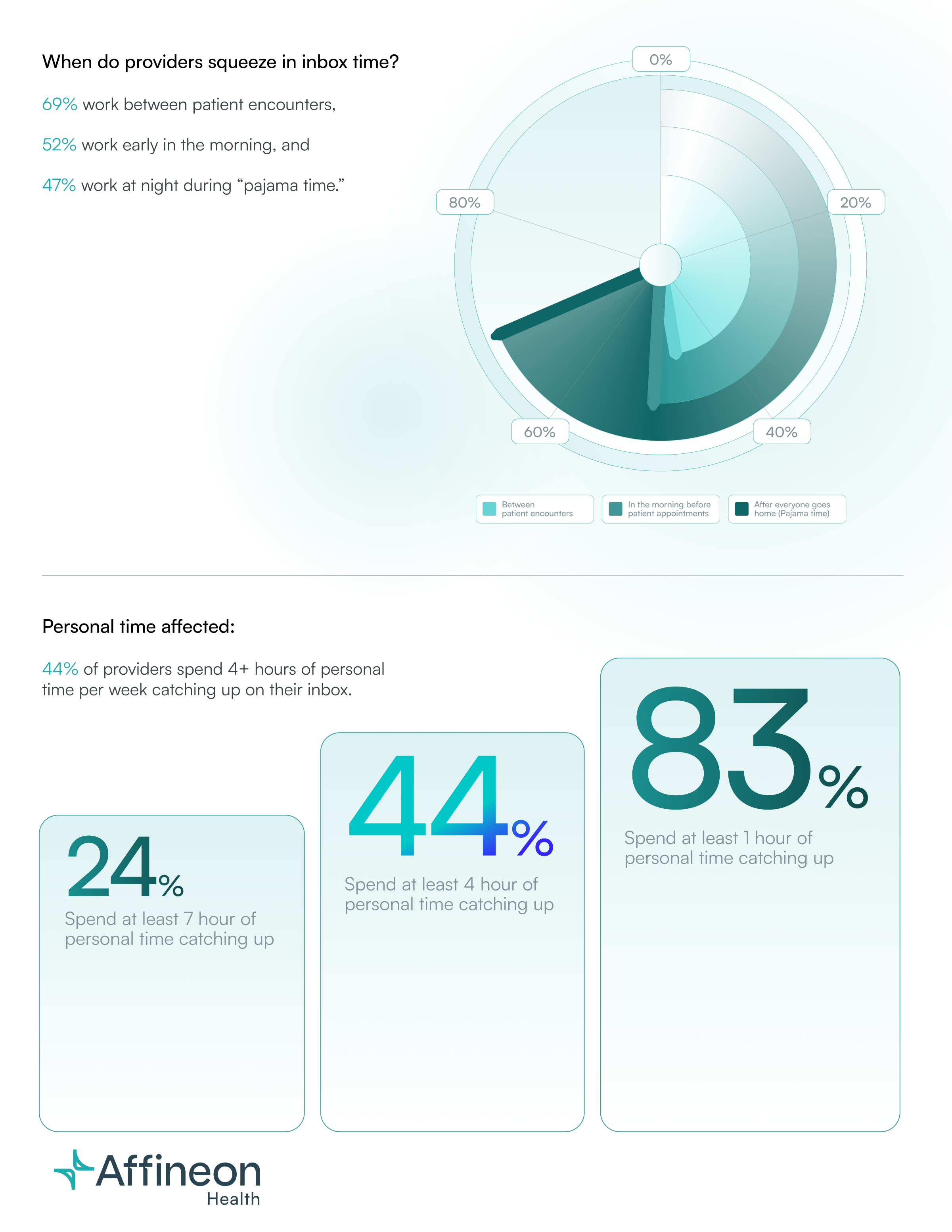
When the last patient leaves, the work keeps coming. The clinic grows quiet, but the inbox stays full. Routine follow-ups and quick checks can swell into hours of catch-up. The sense of never catching up becomes its own kind of fatigue.
The experience Dr. Ryan describes is not isolated. It reflects a national trend that has quietly reshaped the day-to-day reality of clinical work.
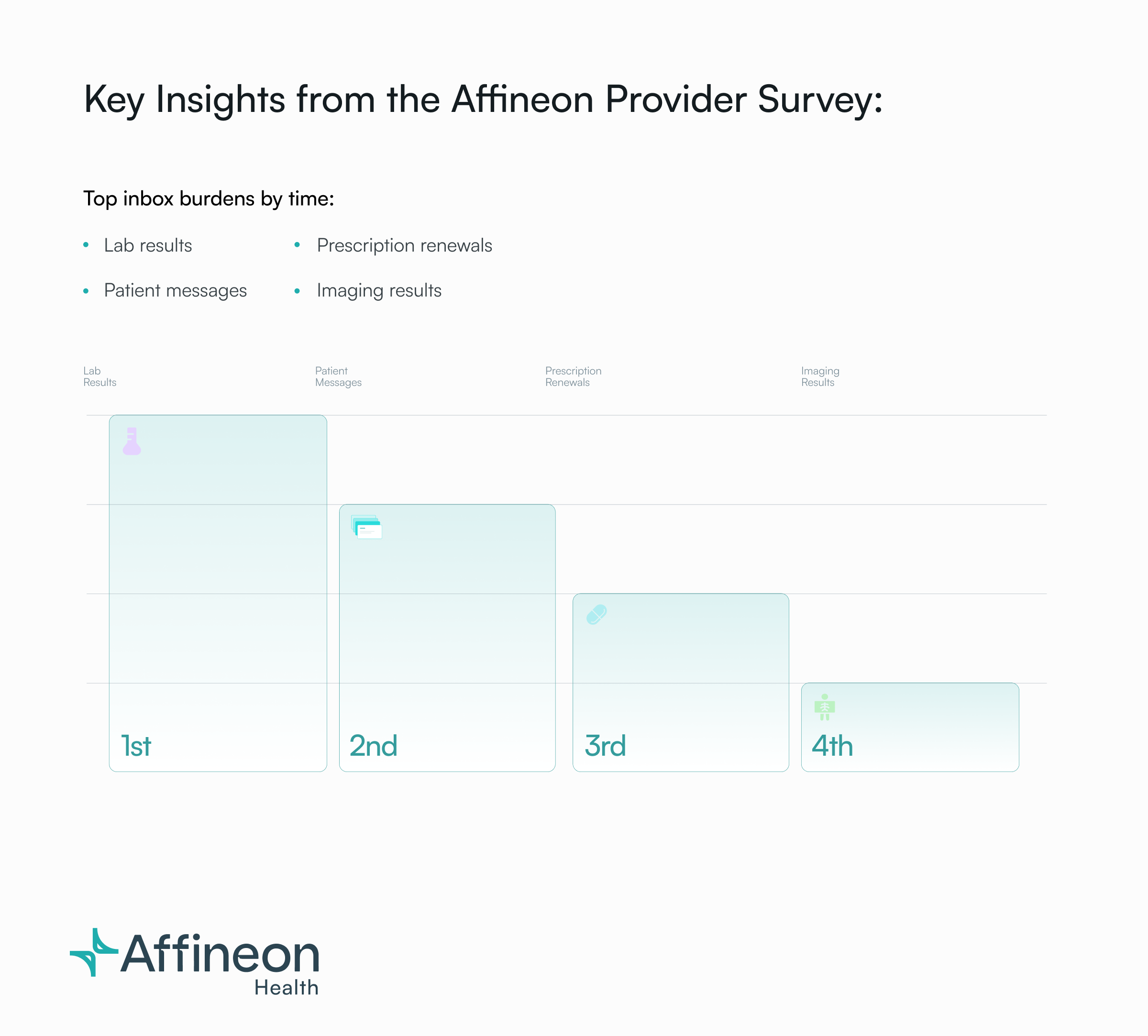
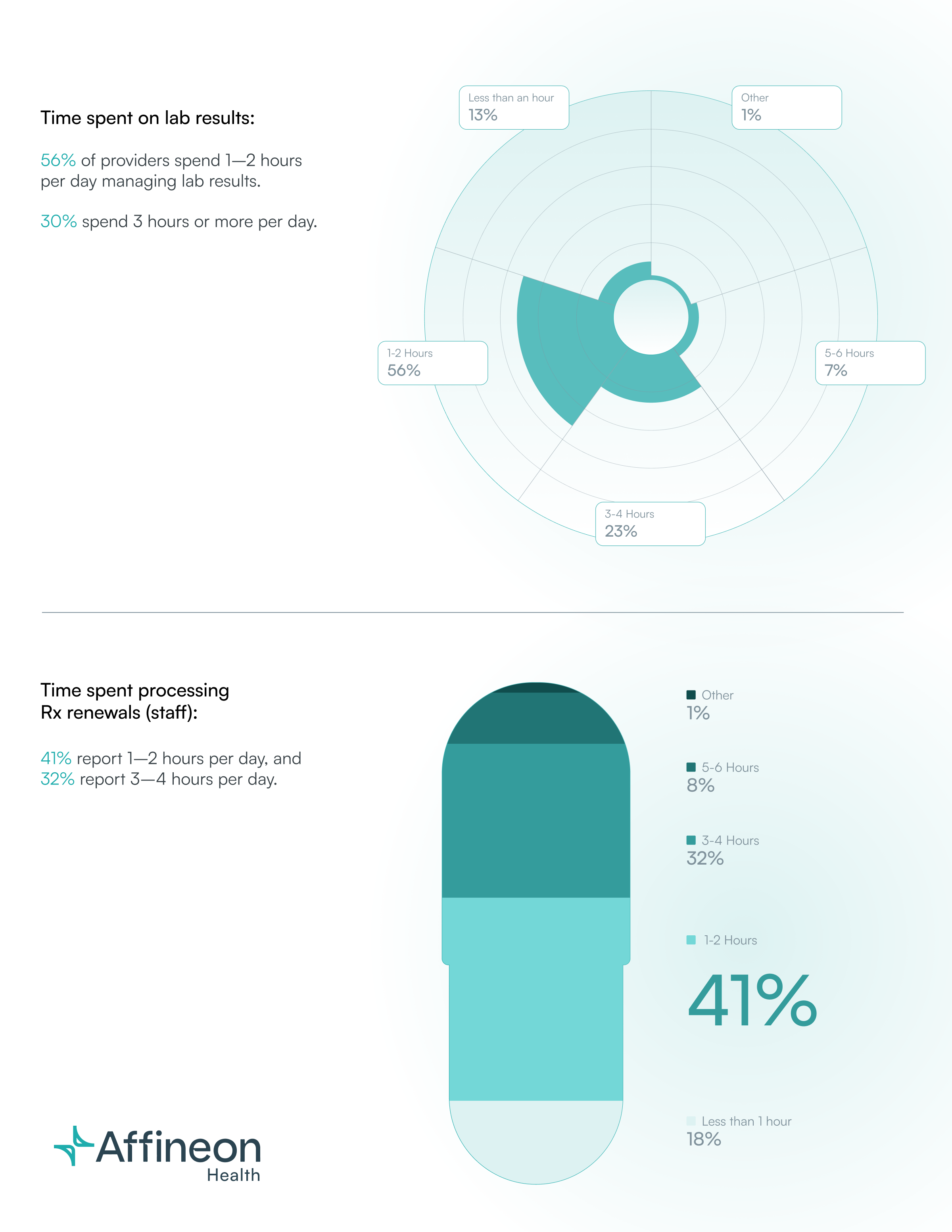
To better understand the scope and specifics of this burden, Affineon conducted a national survey of primary care providers and specialists in the spring of 2025.
The findings are eye-opening. They confirm what many providers and clinical leaders already suspect: the inbox is not just a workflow issue—it’s a serious threat to provider well-being, retention, and quality of care.
But they also point to real opportunities for change. In this report, we highlight the most revealing insights from our survey of primary care physicians and what they mean for practices and health systems that want to scale without compromise while building toward a more sustainable clinical model. Understanding the numbers behind that fatigue was essential. Quantifying the problem made it possible to identify where technology could meaningfully reduce the burden instead of adding to it.
Behind the numbers are stories of clinicians doing their best to keep pace with digital workflows that were built for efficiency, not ease. Many respondents described spending more time in their EHRs than with patients, often logging back in after hours to manage the volume of messages, results, and follow-ups that accumulate throughout the day.

The Role of the EHR Inbox in Driving Provider Burnout
The introduction of electronic health records (EHRs) was heralded as a transformative step toward streamlined, efficient, and safer healthcare delivery.
However, as their adoption became widespread—rising from 18% in 2001 to nearly 86% by 2017 (source)—the unintended consequences began to surface.
Physicians found themselves spending more time navigating complex interfaces and managing digital documentation than engaging directly with patients. This shift not only disrupted the provider-patient relationship but also contributed to a growing sense of dissatisfaction and burnout among healthcare providers.
While EHRs have improved documentation accuracy and access to information, they’ve also created an environment where every task generates a notification. The inbox became the center of that ecosystem—an unrelenting stream of messages that mirrors the complexity of care itself but offers little help in managing it.
A significant contributor to this burnout is the overwhelming volume of messages in the EHR inbox. Studies have shown that physicians with high message volumes are four times more likely to report symptoms of burnout compared to those with fewer messages (source). The constant influx of notifications, many of which are administrative or redundant, adds to the cognitive load and detracts from time that could be spent with patients.
A 2023 longitudinal study of primary care physicians found that since the pre-pandemic era, time spent managing the inbox has jumped by over 20%. From 2019 to 2023, PCPs’ weekly inbox time increased ~24%, and even though it plateaued slightly in the last year, it remains substantially higher than pre-2020 levels. The increase in inbox time has reshaped how clinical days unfold. Tasks that were once delegated or handled asynchronously now land directly in the physician’s queue, often without clear prioritization. Each alert competes for attention, and even brief reviews require mental context-switching that drains focus over time. Over the course of a week, that constant context-switching can add hours of invisible labor and leave physicians mentally spent before the workday ends.
The same study noted a 57% surge in patient messages during the COVID-19 pandemic (as patients turned to portal messaging when in-person visits were limited), and message volumes have stayed elevated ever since. Clinical inboxes were meant to streamline care, but they’ve become digital landfills. Lab results, prescription renewals, patient messages, imaging reports—hundreds of notifications a day, many of which don’t require clinical judgment but still demand attention.
The problem isn’t just about efficiency—it’s about restoring meaning to the work that providers do.
The data makes the scale of the problem clear. But understanding where the friction starts requires a closer look at the workflows themselves.
What’s Broken With Current Clinical Inbox Workflows
Looking at today’s clinical inbox workflows, several systemic issues emerge as fuel for the clinician burnout fire:
Overflowing Inboxes with Low-Value Messages: Too often, physicians are the default recipient of all sorts of notifications. From normal lab results to FYI updates, many of which don’t require their clinical expertise or even attention. The practice of routinely CC’ing physicians on every communication leads to inbox overload, where important messages can get buried. One study found a major contributor to inbox clutter is the lack of filtering: everything from appointment reminders to auto-generated results flows to the doctor. The signal-to-noise ratio in the inbox is poor, and physicians end up wading through hundreds of messages a week, many of which are trivial or could be handled by others. Even with message rules and folders in place, the burden remains because the system still routes responsibility upward. The inbox becomes a catch-all instead of a triage tool.
Inefficient Results Handling: In many systems, when a lab result comes in, multiple people might get notified. If Dr. Grey ordered a test but Dr. Davis is the primary care physician, both might receive it. The redundant notification creates confusion over ownership. This ambiguity in responsibility for results leads to either double effort (two clinicians checking the same result) or, worse, each assuming the other will act (a safety risk). It also means physicians see a flood of normal and CC’d lab results “for your information,” clogging their inbox. The uncertainty wastes time and attention—two resources already in short supply—and adds quiet anxiety about what might slip through the cracks.
Underuse of Team Members’ Skills: In many practices, medical assistants (MAs), nurses, or clinical pharmacists could handle a significant portion of inbox tasks (e.g., routine rx renewals, normal lab results, vaccine questions) with an understanding of orders or protocols. But old habits and rigid role definitions often keep the physician as the default message recipient and decision-maker for even minor issues. This limits efficiency and growth for everyone involved. It also prevents care teams from fully leveraging their collective expertise.
Unnecessary Documentation and Clicks: EHR usability issues force physicians to perform many click-intensive, repetitive tasks. Whether it’s entering the same data in multiple places, dealing with clunky order entry, or navigating through unintuitive screens, the cognitive load of chart-digging through the EHR design is heavy. Even small inefficiencies, from extra screens to broken shortcuts, create friction that erodes focus and satisfaction over time.
Manual Calculations: Manually calculating patient risk for things such as ASCVD, CKD, and FIB-4 scores forces physicians to repeatedly exit the EHR, tediously re-enter patient data into external calculators, and bear the heavy cognitive load of ensuring accuracy—all while risking manual errors and relying on calculators that may be outdated. This fragmented workflow disrupts patient care, wastes valuable time, and introduces unnecessary clinical risk. Repeated manual entry disrupts clinical focus and introduces opportunities for error with every transition between tools.
“No Coverage” Culture: When physicians take time off, their inboxes often wait for them, leading to a dreaded catch-up onslaught upon return. Many doctors check their inbox while on vacation or come back from vacation to hundreds of messages that accumulated in their absence. This creates a sense that one can never truly unplug without paying the price later. Without structured coverage or redistribution of work, time off becomes another form of deferred labor rather than true recovery.
In summary, the current state in many organizations is a default of physician-centric, manual workflows: the provider as the primary processor of all incoming information and the chief scribe for all aspects of care, navigating an EHR that adds friction at each step. It’s a recipe for provider burnout. But it doesn’t have to be this way. The same systems that created this burden can also be redesigned to relieve it through smarter task distribution and better alignment between technology and clinical judgment.

How Affineon’s AI Inbox Agent Relieves Inbox Stress
Affineon is like having a medical assistant that never sleeps, never misses a message, and thinks like a physician. Our AI inbox agent automatically handles normal, insignificantly abnormal, and CC’d lab results, clearing the noise and reducing daily inbox volume by 40-60% and saving providers and their care teams each an average of 5 hours per week. That time goes back to what matters most—direct patient care and the space to disconnect at day’s end.
For lab results that require clinical attention, Affineon does the heavy lifting: we group them, trend them, and summarize them into clean, digestible internal notes that surface the most critical insights for providers at the top of the patient chart. So there’s no need to click around. The result is a clearer picture with fewer distractions—clinical decision-making without the digital clutter.
Affineon also performs smart calculations in the background — including ASCVD, CKD, FIB-4 and KFRE risk scores — and displays them right inside the EHR, so providers never need to leave the inbox or pull out a calculator to determine clinical significance. By integrating these tasks directly into the workflow, Affineon eliminates the small interruptions that compound into hours of lost focus.
Most importantly, providers stay in full control. Every lab and prescription renewal protocol and every patient message is customizable to match how each practice operates. That flexibility ensures Affineon adapts to the practice, not the other way around.
Read more about how Dr. Painter uses Affineon to turn burnout into balance and regain personal time, or how Dr. Abraham uses Affineon to cut his inbox workload in half.